How Good Is Your Heart? Or are your Genes in your way?
By Dr Catherine W Dunne MSc. D., RGN, Reiki Master (RGMT), M.H.I.T: Master Acupressure, Practitioner of Reflexology, Aromatherapy, Deep Tissue/Myo-fascia Massages, Infrared Treatments, Vibrational Sound and Colour Therapist, Tissue Salt Advisor, Pendulum Healing Dowser, Chakra Practitioner , Tao Cosmic Healing Practitioner, Practitioner of Plant and Herb Medicine and Nurse.
Disclaimer: this article I have translated from German to English. In Germany and in USA, they are conducting research regarding best cholesterol lowering treatment, by focusing on Lipoprotein-a. Lipoprotein-a is the cause of fatty livers and the clogging up your coronary arteries. This research is still ongoing with very good outlook. The result is that we may only need a once per annum treatment. Sounds good to me, we’ll see.
Meanwhile, I stumbled across this German article and find it interesting enough to translate for you and share with you.
I hope you will enjoy the read.
Catherine.
Naturally lower Lipoprotein-a
Lipoprotein-a, a relative of cholesterol, is increasingly measured during medical examinations. The lipoprotein-a value is even more important than cholesterol levels when it comes to avoiding cardiovascular disease, they say. We explain how you can lower your lipoprotein-a naturally.
Author: Carina Rehberg
Specialist examination: Gert Dorschner
Current:14 August 2024
Naturally lower lipoprotein
Lipoprotein-A – often abbreviated to Lp(a) – is mainly formed in the liver and consists of 2 proteins, apoliprotein A and apolipoprotein B. It belongs to the blood lipids and is related to LDL cholesterol.
Lp(a) is intended to contribute to the development of Arteriosclerosis and have a prothrombotic effect, which means that it promotes thrombosis (blood clots). Therefore, an Lp(a) value that is as healthy as possible would be ideal. There are hardly any drugs that lower the Lp(a) value. We explain how you can naturally lower your Lp(a) level and thus also reduce your cardiovascular risk.
How lipoprotein-a damages the vessels
Lp(a) damages the vessels and promotes arteriosclerosis as follows ( 1 ):
- Promotes inflammation
- Penetrates the arterial wall, thus enlarging the lesions (injuries) of the vessel walls, which aggravates atherosclerosis
- Attaches more strongly to the blood vessel walls than LDL cholesterol
- Interferes with the formation of plasmin, an enzyme that would dissolve blood clots
Lipoprotein levels: Which ones are good, which ones are bad?
Lipoprotein-A levels should not exceed 25 – 30 mg/dl (for us in Ireland and UK this translates to 0.06-0.08mmol/L. Another example: if your total cholesterol is 6.4 mmol/L this converts to: 247.5mg/dl). If you have higher values (they can rise to 400 mg/dl (10.3 mmol/L) and more), then you assume a massively increased risk of cardiovascular disease, namely for :

- coronary artery disease (blocked coronary arteries)
- Stroke
- peripheral arterial occlusive disease (intermittent claudication)
- Aneurysm of the main aorta – An aneurysm is an abnormal bulge or ballooning in the wall of a blood vessel
- Aortic valve calcification
- Venous thromboembolism – Venous thromboembolism (VTE) is a condition that occurs when a blood clot forms in a vein. VTE includes deep vein thrombosis (DVT) and pulmonary embolism (PE). DVT occurs when a blood clot forms in a deep vein, usually in the lower leg, thigh, or pelvis.
With values above 120 mg/dl (3.1mmol/L), the risk is said to increase 3.6-fold.
Are high Lp(a) values genetically determined?
The personal Lp(a) value is considered to be genetically determined and can neither ne influenced on in any direction – neither upwards nor downwards. So even if the Lp(a) level is too high, it is said that this is “predisposition”. It can therefore hardly be reduced by a change in diet or other lifestyle changes (sports, stress management, weight loss).
Nevertheless, it is precisely these measures that are important even in the case of an elevated Lp(a) value. This is because the cardiovascular risk is particularly increased if there is at least one other risk factor.
So even if your Lp(a) value cannot be influenced, you should do everything you can to avoid any other risk factors (no smoking, no obesity, no diabetes, no high blood pressure, relatively good cholesterol levels, plenty of exercise, healthy eating, etc.). (1).
What factors can increase the Lp(a) value?
Even though Lp(a) levels are considered to be genetically determined, there are some factors that can increase Lp(a) levels – namely some conditions, such as Hypothyroidism (underactive thyroid), kidney disease and a Diabetes mellitus (Type 2 Diabetes(1).
If the Lp(a) level is now elevated due to such a disease, it can of course also be lowered if the causative disease can be alleviated. In the links above you will find measures that help with hypothyroidism and measures that help with diabetes (you may want to set your search engine to translate those pages for you).
Medications that lower Lp(a) levels
There are hardly any drugs that can lower the Lp(a) level and even if they do, they often do not lower the level low enough to reduce the cardiovascular risk. PCSK9 inhibitors (PCSK9 inhibitors are a type of cholesterol-lowering drug. They reduce your levels of low-density lipoprotein (LDL) cholesterol, or “bad” cholesterol.), for example, are used to lower cholesterol, but can also lower lipoprotein-a somewhat, but only by 30 to 40 percent.
PCSK9 inhibitors include the active ingredients alirocumab (Praluent), evolocumab (Repatha) and inclisiran (Leqvio), which are injected subcutaneously for 14 days or monthly. The drugs are very new (maximum approval in 2015), so that side effects are not yet fully known.
Pain and redness often occur at the injection site. However, it can also cause upper respiratory tract infections, itching (pruritus), headaches, joint pain, nausea, aching arms or legs, and fatigue.
The drug AKCEA-APO(a)-L Rx (pelacarsen), which also has to be injected – and in a placebo-controlled study achieved an 80 percent reduction in lipoprotein when administered 20 mg weekly ( 2 ).
Cardiovascular patients or high-risk patients are often given statins to reduce cholesterol levels. However, there are conflicting results on the effect of statins on lipoprotein levels. In two studies from 2016 and 2017, lipoprotein levels even increased at the beginning of statin therapy (1).
In any case, it is important that you know that lowering Lp(a) levels does not necessarily reduce cardiovascular risk (as there are simply too many risk factors for this).
So, you can’t say that we are now lowering the lipoprotein-a value by all means and are then protected from cardiovascular diseases. Therefore, we always point out a holistic approach and advise against always concentrating only on certain values that you now absolutely want to influence.
Lowering lipoprotein – natural remedies
A 2019 study looked at whether natural remedies or supplements known to lower LDL cholesterol levels could also affect lipoprotein levels (1):
- L-Carnitine
- Coenzyme Q10
- Red Rice Yeast
- Pectin
- Ginkgo Biloba
- Linseed
- Curcumin
- Coffee
- Vitamin D
A number of remedies actually had a correspondingly positive effect. Nevertheless, the reduction was not so great for any of the preparations that – if a really high level was present – harmless values could be achieved. It is possible that a more significant reduction in the values could be achieved by combining several natural remedies, but this has not (yet) been investigated to our knowledge.
In the following studies, it is repeatedly recommended to combine the aforementioned remedies with blood lipid-lowering drugs, which should of course be discussed with the doctor.
L‐Carnitin
L-carnitine is produced in the organism from the amino acids lysine and methionine. The substance is particularly involved in the production of energy from fatty acids (which is important for the adult heart, for example) and is therefore also referred to as a fat burner in some places. It is possible that L-carnitine can inhibit the formation of lipoprotein-a in the liver.
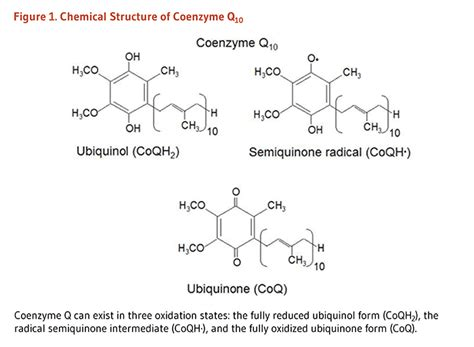
Coenzyme Q10
According to a meta-analysis from 2016, coenzyme Q10 can also reduce lipoprotein somewhat – by 12.5 to over 30 percent (by up to 11 mg/dl (0.3mmol/L)) when taking 120 to 300 mg daily over a period of 4 to 12 weeks. For the analysis, 6 studies with a total of 409 patients were examined. All patients suffered from lipid metabolism disorders.
Q10 doses of less than 150 mg were able to reduce Lp(a) levels more significantly than doses above 150 mg. The higher the original values, the better the patients responded to Q10. Other blood lipid levels, such as LDL cholesterol, HDL cholesterol or triglycerides, were not affected by Q10 intake.
Since Q10 is also used in naturopathic medicine against Side effects of statins if you have to take statins, you can also combine it very well with them and achieve a double goal (fewer side effects and a decreasing Lp(a) level).
- Here is a link to my article on CoQ10
Red Rice Yeast
In a randomized placebo-controlled trial from 2003, patients (with coronary artery disease) were given 1.2 g of red yeast rice per day for 6 weeks and experienced a 23 percent reduction in lipoprotein.
However, red yeast rice extract is not a blank slate, but basically contains nothing more than a natural statin (lovastatin) – and can therefore also have statin-like side effects. It is only less concentrated, therefore better tolerated, so it has a lower risk of side effects.
Statin-related side effects can be reduced by taking coenzyme Q10 – see the section on coenzyme Q10 – so if you want to try red yeast rice, it is best to take coenzyme Q10 as well.
Blood lipids are reduced by red yeast rice because it suppresses cholesterol formation – by inhibiting the so-called HMG‐CoA reductase. It is precisely through this mechanism of action that statins also act.
Pectin
Pectin is a soluble fiber that is abundant in apples or citrus peels. Because pectin has such good gelling abilities, it is also used to boil down jam.
As a dietary supplement, it has long been known to lower cholesterol – presumably because it promotes the breakdown of cholesterol in the liver, but also because it could inhibit the absorption of cholesterol and bile acids in the intestine. (If bile acid is not absorbed in the intestine, but is drained out with the stool, then the liver produces new bile acid from cholesterol, which then naturally leads to a decrease in cholesterol).
A study from 1999 examined whether pectin could also lower lipoprotein-a. In the placebo-controlled, double-blind study, patients (who suffered from high blood lipid levels) received 15 g of pectin daily (for 4 weeks), after which the level of lipoprotein decreased by up to 27 percent.
Ginkgo Biloba
Extracts from the leaves of Ginkgo biloba are usually used for dizziness, tinnitus or for Alzheimer’s prevention. The main effect of the plant is to promote blood circulation. However, it also has anti-inflammatory, antioxidant and antiatherosclerotic properties. Antiatherosclerotic means counteracting vascular calcification.
In a first clinical study in 2006, for example, the administration of 120 mg of extract twice a day after 2 months was able to reduce lipoprotein by 23.4 percent or an average of 10.4 mg/dl (0.3mmol/L) – presumably due to the inhibitory effect on numerous pro-inflammatory messenger substances (cytokines).
In a 2007 study, ginkgo was even able to reduce atherosclerotic deposits in the blood vessels after 2 months in patients who were to receive a bypass. The same dose was used here as in the 2006 study – in the form of the special ginkgo extract EGb 761®, which is contained in numerous ready-to-use ginkgo preparations ( 4 ).
Linseed
Since fiber is generally considered to lower blood lipids and cholesterol, it should generally be part of a healthy diet for lipid metabolism disorders or an increased cardiovascular risk. Linseed consists of almost a quarter (23 percent) of fiber and is therefore particularly suitable here.
In addition, flaxseed contains certain plant substances with high health potential for the cardiovascular system, such as omega-3 fatty acids (cholesterol-lowering) and Lignans (blood lipid-lowering, antioxidant, anti-cancer in breast cancer and prostate cancer).
In a double-blind crossover study with postmenopausal women from 1998, however, flaxseed showed only a small reduction in lipoprotein levels. After six weeks of taking 38 g of flaxseed daily, the value had fallen by 7.4 percent and by an average of just under 2 mg/dl (0.1mmol/L) (1).
From 2008 comes another study (randomized, controlled, double-blind) in which the subjects were asked to eat 40 g of flaxseed per day for 10 weeks. The lipoprotein value decreased by an average of 14 percent compared to a group of patients who took wheat bran (1).
The reduction in the Lp(a) value is therefore rather small, but combined with the other positive effects of flaxseed on cardiovascular risk, it is quite relevant. For example, the small seeds have been able to slow down the progression of arteriosclerosis in various studies (1).
Curcumin
As curcumin, the active ingredient complex is used in Turmeric denoted. It has a positive effect on triglycerides and cholesterol levels, but also on lipoprotein levels. A 2014 randomized controlled trial found that taking 1g per day (for 8 weeks) increased lipoprotein levels in people with Metabolic Syndrome (Metabolic syndrome is a group of conditions that together raise your risk of coronary heart disease, diabetes, stroke, and other serious health problems.) by almost 10 percent (8 mg/dl (0.2 mmol/L)).
Curcumin has anti-inflammatory and antioxidant properties, among other things, and can also reduce cardiovascular risk and support health through these mechanisms of action.
Coffee
Coffee consumption also influences blood lipid levels – due to at least two active ingredients: kahweol and cafestol. However, the content of these two substances in coffee depends on the method of preparation.
If the coffee is made with a paper filter, the active ingredients are apparently largely removed from the drink, so that it has no influence on cholesterol levels. Coffee prepared without filters, on the other hand, could increase LDL cholesterol levels.
In connection with lipoprotein-a, it seems that short-term coffee consumption reduced plasma lipoprotein levels, while regular coffee consumption is associated with higher levels.
Ginger
In a 2020 study, patients with atherosclerosis took capsules containing 1.6 g of ginger powder daily or capsules containing a placebo. After 8 weeks, two values that are elevated in atherosclerosis had dropped significantly – the value of lipoprotein-a and the hs-CRP value (an inflammatory marker that indicates the condition of the blood vessels and helps to assess the risk of heart attack) ( 5 ). In the 2019 paper (1), it was still said that ginger could not lower lipoprotein-a, which does not seem to be true in every case, so ginger can be very well integrated into an Lp(a)-lowering diet plan.
Vitamin D
In 2017, ( 3 ) was examined how Lp(a) levels are related to vitamin D levels (https://www.sciencedirect.com/science/article/abs/pii/S1443950617300252). Participants were 348 patients who underwent coronary angiography (special X-ray examination of the coronary arteries after contrast agent administration). 212 showed coronary heart disease (calcification of the coronary arteries).
- With Lp(a) ≧ 30mg/dl and vitamin D < 10 ng/ml, the risk of coronary heart disease increased more than 4-fold
- The risk was 1.79 times higher for Lp(a) < 30mg/dl and vitamin D < 10 ng/ml
- The risk was 1.7 timeshigher with Lp(a) ≧ 30mg/dl and vitamin D ≧ 10 ng/ml
In each case compared with patients who had an Lp(a) of less than 30mg/dl and a vitamin D level of more than 10 ng/ml.
The study thus shows that a higher vitamin D level can significantly reduce the cardiovascular risk with a high Lp(a) value! Read all about the correct dosage and Taking vitamin D.
This is also an example of the fact that naturopathic measures may not always be able to lower the lipoprotein level (or not strongly enough), but the cardiovascular risk associated with an increased lipoprotein level can be reduced.
These substances cannot lower lipoprotein
Some natural substances lower LDL cholesterol levels, but not – according to various studies – lipoprotein (1), e.g.
- Berberine
- Brazil nut flour
- Garlic
- Olive oil
- Onions
- Vitamin C
- Soy protein and soy isoflavones
Of course, you can still incorporate these foods into your diet or – in the case of vitamin C – take them as a dietary supplement. After all, these are generally very healthy foods that have many beneficial properties and – even if they cannot specifically lower lipoprotein-a – still reduce the cardiovascular risk, and that’s what matters in the end.
Important note
This article was written on the basis of (at the time of publication) of current studies and reviewed by medical professionals, but may not be used for self-diagnosis or self-treatment, so it does not replace a visit to your doctor. Therefore, always discuss any measure (whether from this or another of our articles) with your doctor first.
Warm Wishes as always,
Catherine (CWD)
21 December 2024, Ireland